Diabetic neuropathy is a condition that affects the nerves of people who have diabetes. Peripheral neuropathy can cause tingling, loss of feeling, and pain in the feet. Those most at risk include diabetics who have uncontrolled blood glucose levels, are older, have had diabetes for many years, or are overweight and smoke. Neuropathy can be prevented and treated by controlling the underlying diabetes and taking precautions to keep the feet healthy and the skin on the feet intact. Injuries such as blisters can lead to more chronic problems and poor outcomes in those who have neuropathy in their feet.
Causes Diabetic Neuropathy
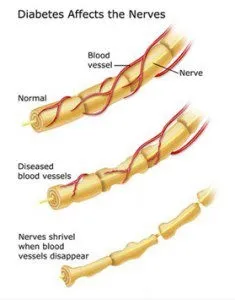
The causes of diabetic neuropathy are poorly understood, but it is likely the result of a combination of several factors. One of the most important factors is uncontrolled diabetes. Diabetes is classified as an auto-immune disease—that is, a disease in which the immune system attacks healthy cells. This abnormal immune response can cause nerve inflammation and lead to symptoms of neuropathy. Nerves may also be affected if damaged blood vessels are not supplying them with sufficient nutrients and oxygen. An individual’s genetic makeup may also play a role.
Risk for Diabetic Neuropathy
Diabetic neuropathy is very common, and 60 to 70 percent of people with diabetes develop the disorder. There are several factors that can increase the risk of developing diabetic neuropathy:
Long-standing disease: Those who have had diabetes for more than 25 years are more at risk for developing neuropathy. After 20 years with diabetes, about 40 percent of people will have neuropathy.
Age: Older individuals who have diabetes are more likely to develop neuropathy than those who are younger. Those over the age of 40 are especially at risk.
Poorly controlled diabetes: Having blood glucose (blood sugar) levels that are frequently too high can increase the risk of neuropathy.
Blood pressure: High blood pressure is more common in people who have diabetes. A blood pressure outside the normal range (higher than 130/80 mm Hg) can cause damage to blood vessels. Damaged blood vessels can contribute to the development of neuropathy.
High cholesterol: People who have diabetes, especially those who have type 2 diabetes, tend to have higher cholesterol levels. Controlling the levels of cholesterol in the blood can help slow the advancement of diabetic neuropathy.
Obesity: Having a BMI (body mass index) greater than 23 can put people with diabetes at risk for diabetic neuropathy.
Symptoms of Diabetic Neuropathy
- Foot pain: Most people with diabetic neuropathy don’t have pain, but for those who do the pain can be intense, and it can worsen while resting. Pain can also be a significant problem at night, which can prevent patients from getting proper rest.
- Tingling in the feet: A tingling or pins-and-needles sensation in the toes is sometimes the first symptom of diabetic neuropathy.
- Numbness in the feet: Numbness can mean an inability to feel temperature changes or pressure in the feet.
- Foot drop: Nerve damage can cause difficulty in working the muscles in the feet while walking. This can result in the foot being raised up high in order to prevent the toes from catching on the ground, and dropping back down with a slap.
Treating Diabetic Neuropathy
Treating diabetic neuropathy in the feet requires close inspection of the feet on a regular basis. Measures must be taken to help the patient cope with pain and control the underlying diabetes.
Foot care: Complications of neuropathy in the feet, such as small injuries, can occur suddenly and quickly become unmanageable. The American Diabetes Association recommends that people with diabetes have their feet examined regularly by a healthcare professional and undergo a comprehensive examination at least once per year. It is also recommended that patients examine their own feet on a daily basis and seek prompt treatment for any injuries, even seemingly minor ones such as blisters. This is particularly true for people with peripheral neuropathy that affects feeling in the feet; an injury that is not painful can still become serious.
Pain control: Peripheral diabetic neuropathy can cause severe pain. In some cases, the pain may start after a change in health status, such as pain that begins during an episode of poor glucose control. The pain may improve without treatment, but this can sometimes take a few weeks to a few months.
Medications are commonly used to treat pain, and several different classes of drugs may be used to control foot pain from diabetic neuropathy. Over-the-counter pain relievers are not effective—and not recommended—for treatment of diabetic neuropathy pain. Different medications may be taken together or alone in order to achieve optimal pain management. Some of these include:
- Cyclic antidepressants: These types of antidepressants are sometimes given to treat diabetic neuropathy pain, but the dosage is much lower than what would be used to treat depression.
- Duloxetine: Another form of antidepressant, Duloxetine is a serotonin-nor epinephrine reuptake inhibitor (SNRI) that has been shown to lessen diabetic neuropathy pain.
- Pregabalin: This anticonvulsant is approved as a first-line treatment for pain from diabetic neuropathy, but it should not be used along with gabapentin. This drug has the potential to be habit-forming and should not be discontinued abruptly.
- Lidocaine: Lidocaine is a topical pain reliever that is administered in a patch form and applied directly to the painful area.
Alpha-lipoic acid (ALA): While alpha-lipoic acid is available over the counter, there is still a lack of good research demonstrating its effectiveness at treating pain from diabetic neuropathy. The effects of its long-term use are not well understood. It is sometimes given to patients who can’t tolerate other treatments, and may be more effective when administered intravenously—but again, good evidence for its efficacy is lacking.
- Narcotics: Opiate-based narcotics are not a first-line therapy for diabetic neuropathy pain, but these medications may be used in the short term while other avenues for pain management are being investigated. Narcotics have the potential to become addictive, and there is always the risk that the patient can overdose.
Controlling diabetes: Because diabetic neuropathy is associated with poor blood glucose control, keeping blood glucose within the appropriate range is important. When a person with diabetes discovers that their current regimen is no longer effective for controlling high blood glucose, the plan should be adjusted by a healthcare professional. Patients should monitor their blood glucose levels carefully, and discuss any changes or difficulty in keeping it under control with their physician. Complications of Neuropathy
Diabetic neuropathy can result in a variety of complications in the feet, and some of them can be very serious, in some cases even requiring amputation. It’s estimated that as many as half of all amputations due to diabetic neuropathy are preventable if feet are cared for properly.
Infection: Even small injuries to the feet can result in infection. Because people with neuropathy can experience a loss of sensation in their feet, they may not realize when they have a sore or a blister. Unnoticed and untreated, even a small sore can develop an infection that quickly becomes troublesome and can invade the bone. An infection that has reached the bone may result in all or part of the foot having to be amputated. Amputations of toes or even the entire foot can be risky for people who are already in poor health, and can result in a person becoming disabled.
Chronic ulcers: Chronic ulceration in the feet is also a major cause of amputation in people who have diabetic neuropathy. Ulcers in the foot require prompt care, including debridement (removal of dead skin) and treatment of any infection. In some cases, however, ulcers do not heal, and remain inflamed. Neuropathy can contribute to this difficulty in healing, especially when it causes blood flow in the feet to be less than optimal.
Preventing Diabetic Neuropathy
Preventing diabetic neuropathy and potential complications means instituting a robust foot-care regimen and controlling the diabetes.
Aside from daily foot inspections and regular foot check-ups from a healthcare professional, good foot care should be practiced. Patients who are at risk for neuropathy or who already have neuropathy should take care in choosing appropriate footwear, avoid activities that might result in foot injury, and learn how to care for long toenails and dry skin. Footwear should not pinch the skin or restrict blood flow, and should have a wide, soft toe box. Any activity that could result in a foot injury should be avoided. This includes not only high-risk activities, but also walking barefoot or exposing the feet to extreme heat or cold. Toenails should be trimmed carefully and filed with a nail file. If necessary, this can be done by a professional instead of at home. Dry skin or any other foot conditions should be managed promptly.
Good control of blood glucose and any other conditions associated with diabetes is also important to preventing diabetic neuropathy. In some cases, when blood glucose is brought to the proper levels, the symptoms of diabetic neuropathy may lessen. Self-checking of blood glucose levels is important, as is following dietary recommendations and medication or insulin schedules. Patients should work with their healthcare providers to learn how to manage high blood glucose levels.



